Vital Signs:
Palladium coils show promise in treating cancer of the prostate
Prostate cancer, like many cancers, can be treated with surgery, chemotherapy, radiation, or various combinations thereof. The implantation of "seeds"—small radioactive particles—into prostate tumors is one common and often effective treatment.
Twist: But a new twist—quite literally—improves on the concept of delivering radiation internally by using a coil instead of seeds. It targets the radioactivity more precisely and thus delivers more to the tumor and less to surrounding tissues. The device was developed with significant input from Dartmouth investigators, and DHMC patients were the first anywhere to receive the new coils.
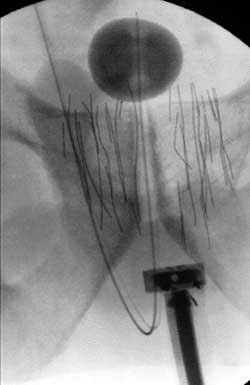 |
| This fluoroscopic image shows a prostate implanted with palladium microcoils (the fine gray lines)—a brand new technology developed at Dartmouth. |
The implantation of conventional seeds involves placing radioactive palladium seeds in a hollow hypodermic needle. Under local or spinal anesthesia, the needle is inserted in the perineal area, the space between the anus and the scrotum, and positioned as carefully as possible using transrectal ultrasound and fluoroscopy visualization. Then the seeds are "planted" in the target area. Scans are taken both before and after implantation to confirm that the seeds have been correctly placed.
This internal approach to delivering radiation is called brachytherapy; the radiation is delivered continuously, over a prolonged period of time, in close proximity to the target tissue. External radiation, by contrast, is delivered in short bursts, at much higher doses, daily over a period of several weeks.
In brachytherapy, however, it is hard to position the radioactive source to both maximize radiation to the tumor and minimize the exposure of adjacent normal tissue. And even with the best positioning techniques, there is always some uncertainty about the precise placement of the seeds; for example, the procedure results in some swelling of the prostate gland, which can change the geometry of the seeds relative to the tumor. And even if the seeds are placed precisely in the beginning, they have a tendency to migrate within the prostate tissue over time. Still, there is a far smaller risk of damage to the urethra, rectum, and bladder with brachytherapy than with external radiation.
So a Boston medical-device company called RadioMed Corporation recently decided to see if there was a better internal option than seeds. The firm turned to DMS to help it develop the concept. From an array of possible shapes—many of them tested experimentally by DMS faculty members Jack Hoopes, D.V.M., Ph.D., and David Gladstone, Sc.D.—RadioMed finally settled on a coil made of palladium.
The device looks like a very fine wire but is actually a microcoil. According to Hoopes, "Coils had two potential advantages over seeds: greater stability after placement in the tissues and improved dosimetry from the long strand versus that of a small sphere."
Testing: First, extensive testing for safety was done in animal models. Hoopes says that dogs suffering from enlargement of the prostate were chosen. "Purebred beagles have a prostate much like humans," he says.
The human first patient received an implanted coil in May 2004, and four of the procedures have been done since then. DHMC is still the only institution in the world using the new microcoils. The coils' availability, however, limits the number of patients who can receive them for the time being, for they must be produced in an experimental reactor in Belgium. RadioMed has plans to build a reactor in the United States, but that solution is several years away.
Future: Also in the future is testing of the coils with other cancers; as is the case with seeds, it is likely that palladium coils can be used to treat tumors in organs other than the prostate. When that happens, DHMC is ideally positioned to carry forward both the experimental and the clinical evaluations of these new applications.
If you would like to offer any feedback about this article, we would welcome getting your comments at DartMed@Dartmouth.edu.
