The profit motive: What does it do to the cost of care?
Is it more economical if hospitals are run on a nonprofit or a forprofit basis? With 192 nonprofit hospitals having converted to for-profit status between 1990 and 1996, that question is far from hypothetical.
On one side of the issue are those who feel that investorowned organizations offer more efficient health care; on the other side are those who think that for-profits are less concerned about quality health care than about keeping stockholders happy. What's the truth?
The truth is there's a lot at stake, and the evidence has been mixed. But an unusual collaboration among three Dartmouth researchers has provided substantial new information, while also stirring up a hornet's nest of controversy. Published in the New England Journal of Medicine, the study found that during a sixyear period, for-profit hospitals billed Medicare more per capita than did nonprofit hospitals. Not only was spending higher in areas dominated by for-profits, but the rate of increase over the years was higher as well.
More costly: "The for-profit hospital service areas were more costly in each year, and that difference actually increased over the six-year period," explains Elaine Silverman, M.D., one of the authors of the study. A general medicine fellow at DMS, she is based at the VA Medical Center in White River Junction, Vt.
Using the Dartmouth Atlas of Health Care and national Medicare data from 1989, 1992, and 1995, the researchers compared overall costs in for-profit, nonprofit, and mixed hospital service areas, as defined by American Hospital Association surveys. After controlling for variables that influence spending —such as age, sex, race, region of the country, number of hospitals, Medicare mortality rate, and number of physicians per capita—they used computer programs to churn out a regression analysis.
Consistent: "Although we may not have measured every little aspect of the hospital service area, we measured three points in time, and it was a consistent finding," explains Silverman.
|
|
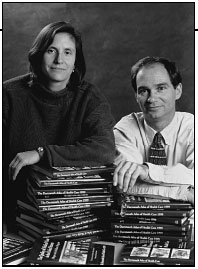
Elaine Silverman, a general medicine fellow at DMS,
and Jonathan Skinner, an economist at Dartmouth College,
pictured here, plus a third colleague, Elliott Fisher,
represent an unusual research collaboration. They
used data in the Dartmouth Atlas of Health Care to
compare costs at for-profit and nonprofit hospitals. |
Because previous research on health-care costs has been indecisive on the question of which are more economical, for-profit or tax-exempt institutions, the Dartmouth researchers decided to ask the question a different way. "Ours is the first study that looked from the perspective of the population," explains Elliott Fisher, M.D., also an author of the study. He and the third author, Jonathan Skinner, an economist at Dartmouth College, had done previous work together on the Dartmouth Atlas.
"Most studies in the past have looked simply at unit cost—the cost per hospital-day or the cost per admission," explains Silverman. "And in fact, most work has found that for-profit hospitals have been more expensive even in that definition, but some have found no difference. . . . The new ground we wanted to address is looking at the population of Medicare patients in a given area and seeing not only what was happening to hospital spending, but spending for home-health services and physician spending in other facilities, such as nursing homes."
What they found was that in 1989, mean, adjusted per-capita spending in for-profit areas was $4,006, or $452 more than in nonprofit areas. By 1995, the forprofit total was $5,172, or $732 more than nonprofits. In each category of service examined— hospital services, physicians' services, home-health care, and services at other facilities—forprofit spending was greater. And in the 33 areas where all hospitals had converted from nonprofit to for-profit ownership, spending grew faster than in the areas where all the hospitals remained nonprofit.
But is it possible that patients received more or better services for the extra cost? The current study wasn't designed to answer that question.
"We can't say whether quality is any different, " says Silverman. "Our best assumption is that there's no difference, in which case they're [just] spending more money, but we'd have to look further to see."
As might be expected, advocates of investor-owned hospitals were not pleased by the study's results, which were immediately spread nationwide by the Wall Street Journal, the Los Angeles Times, Associated Press, and National Public Radio. Critics complained that for-profits were doing better at cost containment than the study indicated.
Taking sides: "Some people come down pretty hard on one side or the other on the role of business in medicine," explains Silverman, who concedes the limitations of the study but confidently defends it against the attacks made by supporters of for-profits. "Although we cannot say from our study the definite mechanism, we can say that in the for-profit areas, all of the costs were higher on average per Medicare enrollee."
Silverman hopes to do more research to shed light on why forprofits are more expensive. She also wants to look more closely at service areas where there are both for-profit and nonprofit hospitals, where the cost difference is less clear-cut, and where competition may be playing a constructive role.
The researchers also want to analyze more recent data to find out if spending trends have changed since 1995.
Collaboration: The team has an edge in the fact that it represents an unusual collaboration among the VA Hospital, the Medical School, and the College. The mix of disciplinary expertise and the access to various knowledge bases has fostered a creative atmosphere in which to analyze the thorny questions related to spending.
"I didn't think when I started the fellowship that I'd be working with an economist," says Silverman, who began her fellowship in 1997, after working as a general internist for the Hitchcock Clinic in Concord.
Fisher hopes that communities will take the results of this study to heart and ask some serious questions before embracing for-profit ownership of hospitals. "We see it as a piece of evidence," he cautions, "that might temper people's enthusiasm."
Lee McDavid
If you would like to offer any feedback about this article, we would welcome getting your comments at DartMed@Dartmouth.edu.
