Puzzling over medical mysteries
By Laura Stephenson Carter
Photographs By Jon Gilbert Fox
|
|
Jonathan Ross has been presiding over the whiteboard at the Department of Medicine's weekly "morbidity and mortality" conference for 15 years. |
Good afternoon," says second-year resident Nathaniel Hare, M.D. This week, it's his turn to relate a "mystery story" to a roomful of physicians, other health-care providers, and medical students at the Department of Medicine's Morbidity and Mortality (M&M) conference.
He'll pause in his narrative every so often, not so much to keep his audience in suspense as to give an opening to anyone who dares to solve the mystery before the end of the hour. But he knows it won't be easy. This is a case that had many of DHMC's top physicians stumped for weeks.
"The cases usually unfold like a puzzle, almost like a good mystery novel," says Donald St. Germain, M.D., acting chair of the Department of Medicine. "Everyone in the audience has the opportunity to be Sherlock Holmes as we look for clues and sort through the evidence."
"The format of the presentation permits the audience to walk in the shoes of the treating physician and struggle to understand what is going on with the patient and what to do at each step as the illness progresses," explains neurologist James Bernat, M.D. "It is educational for all the audience to hear how experienced physicians from a multitude of specialties would care for the patient at each step of the illness."
|
M&Ms are especially educational for the residents— they get "to watch experts with years of experience openly wrestle with difficult clinical problems," says pulmonologist Worth Parker, M.D., who in his role as director of graduate medical education oversees all of the residency programs at the Medical Center. "It gives the residents the feeling that everything isn't black and white."
"What makes it so good is that attendings from all specialties get together in one room to mentally work through a complicated case," says third-year resident Michael Tamber, M.D., who did a recent M&M presentation about an elderly woman who turned out to have a disease that usually afflicts children.
In order for residency programs to be approved by the Accreditation Council for Graduate Medical Education (ACGME), they must have a quality assurance (QA) process, explains Parker. "It takes an honest give and take regarding things that go well, and things that don't, for quality improvement to occur."
M&M conferences represent one form of clinical QA activities. Patient complications and deaths are discussed for the purpose of educating staff, residents, and medical students. State statute protects the discussions of what might have gone wrong. "By having this protection in place, it is believed that clinicians will be open and honest when things do go wrong, so that we can learn from them and improve," says Lisabeth Maloney, M.D., an anesthesiologist and DHMC's executive medical director.
In many departments, M&Ms tend to focus on what went wrong with the way a patient's care was managed. At DHMC, although "the Department of Medicine's M&Ms fits the criteria for QA, . . . it's sort of a hybrid," explains Parker. It's a mixture of an interesting-case presentation and of a true M&M conference.
A long tradition
M&M conferences have a long tradition in the practice of medicine, having originated in the early 1900s at Massachusetts General Hospital in Boston. "Ernest Codman was the first surgeon to start M&Ms," says John Birkmeyer, M.D., chief of general surgery at DHMC. "He was father of the efforts to apply a systematic approach to tracking patient outcomes after surgery." A framed copy of one of Codman's outcomes charts hangs on the wall in Birkmeyer's office.
|
Codman's ideas contributed to the standardization of hospital practices—including a case report system that ascribed responsibility for adverse outcomes— by the American College of Surgeons in 1916. As the medical profession evolved, physicians grew accustomed to discussing their errors at mortality conferences, where autopsy findings were presented, and in published case reports. By 1983, the ACGME began requiring that accredited residency programs conduct a weekly review of all complications and deaths.
But DHMC was running M&M conferences long before ACGME made them a requirement for residency accreditation. Many attribute the popularity and success of the Department of Medicine's M&Ms to Jonathan Ross, M.D., who has been the director and moderator of the conference for 15 years. "Jonathan Ross creates a very safe environment for faculty to air their opinions, and uses humor effectively and backs off early if there's any sense of discomfort," says infectious disease specialist Kathryn Kirkland, M.D. "It is fun to be able to contribute to learning, to have a dialogue with other physicians, and to have the residents and students see how that can be done in a collegial and comfortable atmosphere."
"The atmosphere is generally supportive," says St. Germain. But, he adds, "it can be a bit daunting to speak up in front of a room of experts and offer an opinion that you know might get blown out of the water with information to be presented on the next slide."
He, too, attributes the success of the M&Ms to Ross's leadership. "He is a superb physician, and his contributions in terms of maintaining the proper pace of the discussion, ensuring the supportive and respectful tone of the conference, and guaranteeing its educational value cannot be overestimated."
And St. Germain credits the chief residents, too, for spending "a huge amount of time behind the scenes. Their contributions to the educational value of the conference are hidden from view, but substantial indeed."

|
|
John Birkmeyer, chief of general surgery at DHMC, is a disciple of Ernest Codman, who originated the concept of M&Ms a century ago. Here, Birkmeyer points to an antique Codman outcomes chart that hangs on his office wall. Surgery holds weekly M&Ms, as do other departments, but this article focuses on the M&Ms in the Department of Medicine. |
A lot of time and effort go into preparing each case. Ross works with the chief residents and the second- and third-year residents to choose cases and develop engaging and educational presentations. "Case preparation is very time-intensive for the residents, and they do the lion's share," says Ross. "I do the final editing after meeting with them."
For this day's presentation, Nathaniel Hare and chief resident David Feltquate, M.D, had met with Ross the week before to discuss the case and polish the presentation.
"Usually we will have gone through a couple of drafts and then we'll sit down and go over it with Dr. Ross," Feltquate explains. "Then we'll talk about things that need to be changed, any major holes, and then talk about the teaching aspects— what kinds of lessons do you want to communicate to people. What are some of the questions that we want to tease out of the audience and get them to be talking about."
"What kinds of things do you think you would like the audience to come away with?" Ross asked Hare. "Is it the 'golly gee' effect? An unusual case? Is it an interesting pathophysiology? Or differential diagnosis?"
"I think differential diagnosis," Hare replied. "I think one of the things for me was sorting out what's the differential for somebody that sounds like they presented with a viral rash." A "differential diagnosis" is the process of distinguishing among two or more similar diseases by systematically comparing their signs and symptoms.
"This sounds good," Ross told Hare after they'd spent about 30 minutes fine-tuning the complicated presentation. They'd eliminated some details so as to avoid overwhelming the audience, but they hoped they had preserved enough to tell a compelling, and educational, story. "This is clearly a case that challenged the best minds in the institution for a month."
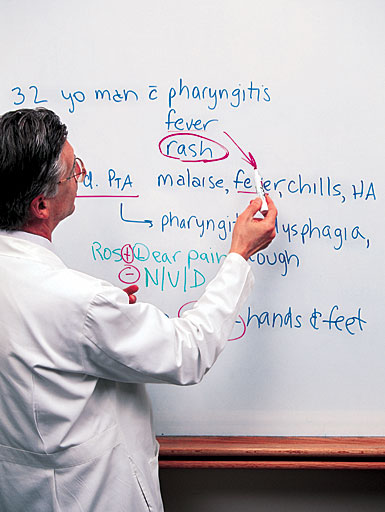
Malaise, fever, chills
Hare begins. "A 32-year-old white male presented to an outside hospital for evaluation of sore throat, fever, and a rash. He had been in his usual state of health until three days prior to admission. He developed malaise, fever, chills, and a headache. Later that same day he developed a sore throat, difficulty swallowing, a nonproductive cough, muscle aches, and watery stools. The day prior to presentation he developed a rash on his hands and feet, which then spread to his trunk and the rest of his body. The rash did not itch. It occurred after taking Contac, an over-the-counter cold medicine that is a combination of pseudoephedrine and acetaminophen. The patient reported swollen glands in his neck, with mild neck stiffness, as well as left ear pain. Of note, he denied vision or hearing problems, nausea or vomiting, chest pain, shortness of breath, abdominal pain, blood in his stool, urination difficulties, joint pain or stiffness, itching, recent travel, or any sick contacts."
|
As he speaks, Hare is operating a computer keyboard to change the slides projected on a giant screen behind him. Years ago, residents would have had to use overhead transparencies and slide projectors to show the text and the radiology and pathology studies that accompanied their presentations. But nowadays, they use PowerPoint computer software to integrate text with digitized radiology and pathology images, photographs, and even videos to create a professional-quality presentation.
But it takes more than nice-looking slides to impress this audience. Hare must also demonstrate that he has a mastery of the sophisticated language of medicine, with its vocabulary of technical terms, abbreviations, and numerical values that doctors use to convey important information quickly and accurately. He seems to be doing fine so far.
Ross, who has been recording key points about the case on the whiteboard at the front of the room, interrupts to ask the audience, "What kind of thoughts come to mind as to what might be going on?" He looks at one of the pulmonologists and asks, "Your average, everyday case of some respiratory tract infection or . . .?"
"It sounds like he's got a lot of respiratory tract symptoms generally," says the pulmonologist. "I guess the one clue is he has some sort of rash. . . . So it sounds like he's got, most likely, some sort of acute infection."
"Other initial thoughts? This is the walk-in clinic kind of patient," Ross reminds the audience.
"Scarlet fever?" a gastroenterologist volunteers. "Had he had indigestion?"
"I don't think he had that," says Ross, nodding for Hare to continue.
Hare then describes the patient's past medical history, his family's medical history, and his social history. He had nothing "remarkable" (that is, medically significant) to report.
"The physical exam revealed an elevated temperature, hypotension, tachycardia, and hypoxia," Hare says. Translation: the patient had a fever and low blood pressure, his heart was racing at more than 100 beats per minute, and he wasn't getting enough oxygen.

|
Acute renal failure— that is, kidney failure — is unlikely, responds the nephrologist; the patient's creatinine level is not too high for someone so muscular. . . . An infectious disease expert wonders aloud if anthrax should be considered in the mix of possibilities. "So the diagnoses are getting more and more sinister as this case goes on," says Ross. |

| |

|
The blood tests showed a high white blood cell count, suggesting that an infection was present. Other lab results were abnormal, too, suggesting a possible kidney problem. "The emergency room physician was concerned that the patient might have meningitis, so a lumbar puncture was performed," says Hare. A lumbar puncture, also known as a spinal tap, is an invasive diagnostic test in which cerebrospinal fluid (CSF) is extracted for examination for signs of infection.
But "the CSF labs were normal," Hare continues. Tests for strep throat and mononucleosis were also negative, and the patient's "chest x-ray was read as clear."
A kidney connection
A specialist in infectious diseases wonders whether the patient is showing signs of early sepsis. Sepsis is an overwhelming infection in the bloodstream caused by toxin-producing bacteria. A nephrologist is concerned about HIV infection.
"Why do you think he doesn't sound sick enough for acute renal failure?" the pulmonologist asks the nephrologist. "He's hypotensive, tachycardic, and has got an O2 requirement."
Acute renal failure—that is, kidney failure—is unlikely, responds the nephrologist. The patient is young and his creatinine level is not too high for someone so muscular. Creatinine, a protein produced by the muscles and released into the blood, is an indicator of kidney function.
Someone's pager begins beeping, sending a physician scurrying from the room. No one seems to notice as pagers chirp and physicians come and go during the hour-long conference. Everyone else stays focused on the presentation; even those who leave the room and return have managed not to lose track of the discussion.

|
|
Jonathan Ross (left) spends time before each M&M session, helping the resident who will present that week's case figure out what elements should be included and how the presentation should unfold. Here, he discusses the case that is the subject of this article with Nathaniel Hare, who is a second-year resident in internal medicine's primary-care track. |
"Does acute HIV give you hypotension?" a pharmacologist asks the infectious disease doctor.
"Not that I know of," says the infectious disease expert. "It's more sort of severe flu-like, but I think that's a reasonable thought."
The pulmonologist speaks up again. "I think I'd move beyond early sepsis syndrome. . . . He's got sepsis and organ dysfunction. He's well along. I'd cross out the early."
"Okay," says Ross as he crosses out the word 'early' that he'd written on the whiteboard.
Another physician wants to know, "What time of year was the presentation?"
"February," Hare replies.
"So it's probably not a tick-borne disease," says the doctor.
Unfolding story
As the story unfolds, the audience learns that the patient was admitted to the local hospital and treated with intravenous fluids for hypotension, but his blood pressure kept dropping. "In the middle of the night he was transferred to the intensive care unit for better management of his blood pressures," says Hare. "The internist caring for him felt that the patient most likely had a viral syndrome with a reactive rash, and a second chest x-ray was obtained."
Next, chief radiology resident Fayyaz Barodawala, M.D., comes to the lectern to interpret the chest x-ray that appears on the screen.
Radiology residents—usually whoever is assigned to the musculoskeletal rotation—often digitize the films, review the findings, and discuss them at medicine's M&Ms. Likewise, when there are pathology or autopsy results, someone from pathology reports on them at the medicine M&Ms.
"Here's a cardio-mediastinal silhouette here, and there's widening of the superior and anterior mediastinum," Barodawala explains. The mediastinum is the area in the middle of the chest, between the lungs. "If this was a trauma patient, obviously we'd be concerned about aortic injury. . . . Given he's a young guy, I think of lymphoma or reactive adenopathy [gland enlargement], or an abscess."
|
As Barodawala leaves the lectern, an infectious disease expert wonders aloud whether anthrax should be considered in the mix of possibilities. "So the diagnoses are getting more and more sinister as this case goes on," says Ross.
Hare continues to reveal the clues as they presented themselves during the case. The internists at the local hospital thought the patient had a viral syndrome with a reactive rash, but the infectious disease specialists there were concerned about the possibility of an overwhelming bacterial infection. Strangely, though, the blood cultures were negative. The patient was started on intravenous antibiotics— Azithromycin, Ceftriaxone—and a steroid—Solumedrol. A CT scan shows lymphadenopathy (swelling of the lymph nodes) in the patient's neck and chest and "a possible mediastinum phlegmon." A phlegmon is an inflammation of the connective tissue. "Infectious disease felt that this represented a neck infection with mediastinal extension," says Hare. "Clindamycin was started and the patient was transferred to the Dartmouth- Hitchcock Medical Center ICU."
Appropriate antibiotics
Ross asks the audience to comment on whether the appropriate antibiotics had been prescribed.
"It seems like the infection was rapidly evolving, so that was good initial coverage," says the infectious disease (ID) expert.
The pulmonologist disagrees. "I'd want my ID person to think long and hard about systemic infections which would involve the mediastinum. Given how ill he is, I'd consider providing coverage for those pathogens as well."
"The exam at DHMC showed that he was struggling to breathe, with an elevated temperature, hypotension, tachycardia, and hypoxia," Hare continues calmly. Some of the lab test results are abnormal, and the patient's blood gases are out of whack. The carbon dioxide content (which is expressed as PCO2) and the oxygen content (expressed as PO2) of the blood are way below normal. Arterial blood gas measurements are important in the evaluation of cardiac failure, hemorrhage, kidney failure, drug overdose, shock, or other conditions of severe stress.

|
Soon, "infectious disease, cardiothoracic surgery, and cardiology agreed that the patient had fulminant viral myocarditis," explains Hare. Translation: there was a sudden, virally caused inflammation of the myocardium, or heart muscle. "Influenza virus and adenovirus were considered the two most likely causes," Hare continues. |

| |

|
"It sounds like he's got a lung problem," says the pulmonologist. "He's got a PO2 of 56 on 100 percent, so he's got profound impairment in oxygenation. I do think he needs to be intubated. It doesn't sound like he's heading in a good direction."
Respiratory distress
When DHMC assessed the patient, "it was felt that his infection possibly started as influenza," Hare explains. "Now the patient had likely developed a bacterial superinfection, with pneumonia as a possibility, plus mediastinal widening and infection. Inhalational anthrax was considered much less likely since he had no known exposure. . . . Empiric antibiotics were started—Clindamycin and Moxi- floxacin. . . . . Over the next few hours, the patient had progressive respiratory distress, prompting the team to electively intubate him."
"What's Moxifloxacin have that others don't?" Ross wants to know.
Before the infectious disease expert can answer, someone stage-whispers, "A lot of moxie," and a few people laugh. The question does get a serious answer, too: "It sounds like they were thinking more about the respiratory infection," says the expert. "It's fine. What needs to happen is a diagnosis needs to be made."
Soon, "infectious disease, cardiothoracic surgery, and cardiology agreed that the patient had fulminant viral myocarditis," explains Hare. Translation: there was a sudden, virally caused inflammation of the myocardium, or heart muscle.
"Influenza virus and adenovirus were considered the two most likely causes," Hare continues. "He did not need surgery at this time but might need an intraaortic balloon pump if his hypotension persisted. Finally, dermatology weighed in. They felt that the patient's rash was consistent with a viral illness versus a drug reaction, with the drug reaction being much less likely."
"So what does the assembled cardiology brain- power here think about this case?" asks Ross. "Is this viral myocarditis?"

|
|
Resident Nathaniel Hare (left) is working here with Ross on the details of his presentation—a process that involves sifting through the entire patient record and then crystallizing the pertinent facts into a computerized PowerPoint slide show. The small photos on the lefthand pages of this article were all taken the day of Hare's actual presentation. |
"Well, it's cardiomyopathy," says one of the cardiologists. Cardiomyopathy refers to any disease that weakens the heart muscle. "Whether or not it's a myocarditis, that hasn't been demonstrated. And a viral etiology would be the most likely. But at that degree of hypotension, I have to wonder what his systemic vascular resistance is, and I'd want to measure that."
"How about a myocardial biopsy?" asks Ross.
"It's not a very useful test in most settings," another cardiologist replies.
The pulmonologist is growing agitated. "You have a fulminant sepsis syndrome rather than simply myocarditis," he says. "We've shown evidence of pulmonary dysfunction, renal dysfunction. He's really got a systemic disease. I think it's kind of a narrow perspective to say he's just got fulminant viral myocarditis. He's got pharyngeal inflammation and a mediastinal inflammation."
Ross turns to one of the nephrologists. "Is it renal inflammation?"
"I'd be inclined to sit down and talk to the ID person and generate a list of organisms that could do this," says the nephrologist. "Then I'd go back to the patient and his family and talk about contacts, anything unusual, any place unusual he's been recently, anything he's done recently. I don't know, fishing somewhere weird. Just to try and get some clue as to what this could be."
"It's February," Ross teases. "We're not fishing anywhere."
"Ice fishing?" counters the nephrologist with a laugh.
Another nephrologist comments. "If you put him on the right antibiotics, it's probably not going to influence his course in the first 48 hours with this kind of sepsis anyway," he says. "It's important to get him on the right antibiotics, but the die is cast and you know now we need to look at some of the newer therapies," including some experimental ones being tried in ICUs.
The pharmacologist agrees with the pulmonologist that the patient is probably "in a very advanced sepsis syndrome. It might be that he's so sick that nothing responds to treatment," says the pharmacologist. "In general, bacteria in an acute setting respond better than viruses. We don't have great drugs for acute viral sepsis-related syndromes, but we do for bacteria. I'm worried that I don't know whether he's got acute viral, acute bacterial, acute fungal, or something like Rocky Mountain spotted fever. It's not the right season for it, but we don't know exactly where his travel was."
|
Hare describes how the patient progressed over the next couple of weeks. On the cardiology front, the patient seemed to be improving. The cardiologists in the audience are not surprised. One says that he would expect this type of myocarditis to "get better as the sepsis resolves."
Pneumonia? Mycoplasma?
On the infectious disease front, the patient spiked daily fevers until his 14th day at DHMC, and his white blood count shot up to 37,000 (the normal range is 5,000 to 10,000) and then subsided slowly. "On hospital day 14," says Hare, "the mycoplasma IgM [a form of immunoglobulin] serology returned positive." One species of mycoplasma, the smallest free-living organism, is known to cause a mild form of pneumonia in people under 40.
"The infectious disease service thought that if this indicated a recent mycoplasma infection, the patient had already been treated appropriately with Moxifloxacin for seven days. However," Hare goes on, "mycoplasma could cause a myocarditis viral syndrome and CNS [central nervous system] infection, and the patient had had signs of all of these." There were other signs that he might also have pneumonia, Hare adds. So the patient was put on Moxifloxacin once again and Ceftazidime "to cover possible pneumonia and to cover him in case he was still infected with mycoplasma."
"Could this be IgM myocarditis syndrome?" Ross asks one of the infectious disease experts.
"That's the big question," responds the infectious disease person. "Everybody was a little surprised that the mycoplasma came back positive. I think I came on service in the aftermath of this. . . . Now that we have this new information, and mycoplasma IgM is a good test, is that relevant to what's been going on or is it not?
"I think that what everybody had a hard time swallowing," the infectious disease specialist continues, "was that mycoplasma isn't supposed to make you this sick. . . . And yet you can go to the literature and find statements that every now and then mycoplasma can cause a fulminant, horrible disease in a young person. The question is 'Okay, is that enough, do we now stop looking and say we have a diagnosis and everything wraps up neatly?' In retrospect, the answer to that question probably was 'Yes.' But at the time I don't think that was the answer."
Polyneuropathy issues
"Well the excitement isn't over," says Ross. "So let's keep going."
On the neurology front, the patient's mental status began to improve once the breathing tube was removed on his 11th day in the hospital. But he was very weak—he needed help to stand—and his upper extremities were even weaker than his lower ones. "A neurology consult on hospital day 13 thought that he had encephalopathy, and . . . infectious disease was thinking that the patient's weakness was due to possible CNS disease versus a polyneuropathy"—a condition where many peripheral nerves are affected with a disorder. By hospital day 17, he was doing so well he was transferred out of the ICU. He also got an MRI of his brain and spinal cord. But later, Hare says, he had "myoclonic jerking of his legs [leg spasms], which resolved with Ativan," an antiseizure drug.

|
"That's the big question," responds the infectious disease expert. "Everybody was a little surprised that the mycoplasma came back positive. I think I came on service in the aftermath of this. . . . Mycoplasma isn't supposed to make you this sick. . . . And yet . . . every now and then mycoplasma can cause a fulminant, horrible disease in a young person." |
 | |
 |
"One of the issues that we always have is critical illness polyneuropathy," explains a neurologist who had been involved in this patient's case. "It's something that just doesn't go away that quickly. What's interesting is when we see someone who has abnormal involuntary movement and you give them Ativan or something like that and it goes away, very high up on one's differential becomes seizures, be it focal or generalized."
Barodawala comes back to the lectern again, ready to interpret the MRI that now appears on the screen. "I picked two selected images from the MRI to show you guys what's going on," he says. "Just of interest, his spinal canal is relatively narrow. You're not seeing a lot of cerebrospinal fluid around it. So you've got some congenital spinal stenosis. We see that sometimes." Otherwise, he concludes, the MRI offered few clues.
But there were still more twists to come in this mystery. On hospital day 18, the patient had a grand mal seizure that "lasted roughly two minutes and was aborted with Ativan," says Hare. "His heart rate was in the 150s to 160s, with his blood pressure in the 130s over 70s. He was transferred back to the ICU and intubated for airway protection, as he was somnolent." ("Somnolent" is medspeak for "drowsy.") "His Moxifloxacin was changed to Azithromycin, as there was concern that Moxi- floxacin could have caused the seizure," Hare adds.
Ross interrupts to ask, "Do we know anything about Moxifloxacin and seizures?"
"Yup, it can cause seizures," says the infectious disease expert.
"So what do we do now?" says Ross. "He seems to have been getting better in some organ systems and now he has seizures. Is it enough to ascribe it to the Moxifloxacin, or do we have to keep looking?"
A neurologist gives a long explanation, but his point boils down to this—Moxifloxacin isn't necessarily to blame for this seizure.
Hare then reports that the differential diagnosis included five possibilities: post-infectious mycoplasma- related encephalitis; systemic illness with encephalopathy, myocarditis, and myopathy (muscle disorders); myopathy from a mixed cryoglobulinemia— the presence of abnormal proteins called cryoglobulins—possibly indicating hepatitis B or C; vasculitis (an inflammation of the blood vessels); or acute HIV.
On day 28 the patient was transferred out of the ICU, and on day 34 he was discharged to home with prescriptions for antiseizure medications and antibiotics. He has since returned for follow-up visits with neurology and infectious disease and seems to be doing well.
The last word
And the final diagnosis?
"Neurology felt that he most likely had a critical illness polymyoneuropathy," says Hare. "Infectious disease felt that he had most likely had a mycoplasma myocarditis complicated by MRSA sepsis"— that is, a toxic infection caused by Methicillin- resistant Staphylococcus aureus.

|
|
After Hare's presentation, Jonathan Ross (right) agrees with David Feltquate (left) and another attendee that Hare did a good job. Feltquate is one of the chief residents in internal medicine, and part of his position includes helping to select the cases that will be presented at each week's M&M and supervising the residents as they develop their presentations. |
Hare also points out that the total bill for this patient was over $200,000. "Since the patient had no medical insurance, the Hospital and Clinic have written off the entire bill," he notes.
"So let's think about this and force ourselves to learn a little bit about this case," says Ross. "What was done well and what could have been done better? We've had an opportunity to immerse ourselves in this very complicated story."
|
"I think a lot of things were done very well," says the infectious disease specialist. "He received immediate ICU care. The housestaff were extremely attentive to this guy throughout the ups and downs of his hospital course and they stuck with rethinking him every few days. It wasn't completely clear whether the newest development was related to the initial diagnosis or not. What could be improved? I think it's not advisable if you can't figure out what someone has to give them a [diagnosis of] nosocomial infection." A nosocomial infection is one acquired during a hospital stay. "This guy really came close to dying of sepsis, and that would have been a real tragedy. As I look back on it from my own standpoint, I think that the diagnosis of mycoplasma was reasonable and that maybe we could have embraced that a little bit more in real time. It might have avoided a series of deviations from the path that didn't necessarily need to be done. It was a dif- ficult diagnosis to make, but I think the myocarditis, even the sepsis syndrome at the beginning, and the mediastinal edema—which is what they ended up calling that—even the polyneuropathy and potential encephalopathy, all could be ascribed to the mycoplasma."
"So how could the Staph aureus have been prevented?" the pulmonologist asks. "Did he have a catheter that was in for an unreasonably long period or is this just an unavoidable risk associated with critical illness?"
"Well, this is the high-risk population in which you expect these infections to occur— in the ICU for a long time, multiple antibiotics, and other lines in place," answers the infectious disease specialist.
"Back to once again what was done well," says someone else. "We've got an otherwise healthy 32-year-old guy who . . . was barely hanging on. We see some trauma patients like this as well—people who are this young but that sick—and they're going to crash very shortly. He probably wouldn't have survived except that he was in the ICU. I think that was a critical decision to put him right in the ICU, not say, 'Well, he's kinda sick, let's watch him out on the floor.' He probably would have died that night. So if you get somebody this young who should be healthy but is this sick, there's only one place they need to be and that's in the ICU."
"On that note, I think we'll stop," says Ross (who reflects on the ritual of M&Ms in the adjacent box). "Thank you very much." The audience applauds in appreciation for an especially interesting presentation.
As people file out of the room, Ross and Feltquate stop to chat with Hare, who is visibly pleased. He says he thought the presentation and discussion went well. And he learned something by being involved with— and presenting—the case. "I learned that the suppression of myocardial function is within the limits of what can be expected for a very sick patient," he said in an e-mail to Dartmouth Medicine a few days later.
But some element of mystery remains still. Although M&M discussions usually contribute to a better understanding of what went on in a case, they don't necessarily answer all the questions. The diagnosis "is about as clear as it will ever be," Hare says. As best he can figure, the patient had "the mycoplasma infection and this was complicated by the sepsis and polyneuropathy. This is as close as I can come to a diagnosis."
Next week it will be another resident's turn to be in the spotlight. And Jonathan Ross will once again host the hour of suspense known as M&M. �
Reflections on M&Ms
By Jonathan Ross, M.D.
Jonathan Ross, an associate professor of medicine and of community and family medicine, has been directing the DHMC Department of Medicine's "Morbidity and Mortality" conference since 1987. He was recently appointed DHMC's Almy Clinical Scholar, a three-year post that is named in honor of the late Thomas Almy, M.D., former chair of medicine.
I have tried to create a safe learning environment in the Department of Medicine's M&M conference: Where faculty can model their humanism, analytic skills, and knowledge for students, residents, and faculty colleagues. Where humor creates a lightness of spirit, even while we grapple with the difficult work of medicine—differential diagnosis, pathophysiology, pharmacotherapeutics, ethical and social issues, end-of-life issues, and cost issues.
It's been a successful conference when many have participated in the discussion, when areas of controversy have been explored openly, when the focus of the discussion comes back to the individual patient, when we have learned from each other.
This is the one conference that serves as an antidote for the fracturing of the department into work zones. When we were back on the Hanover campus we fit the entire department—it was much smaller then—into the old Bowler Auditorium, and we often spoke with each other as we saw patients at Desk 200. As we've grown, the interaction between sections has been reduced. M&M restores a collegiality in problem-solving and connections and models a departmental ethos.

|
|
Jonathan Ross: Internist and director of M&M |
The radiology and pathology departments have provided wonderful support for our conference. Radiology residents discuss the films and offer a differential diagnosis from a radiological standpoint. The pathologists often have the ultimate word in discussing pathology or autopsy findings.
We have searched for ways for the M&Ms to reach a larger audience. Last year, we experimented with digitally recording the conference and placing it on a password-protected portion of the DMS Web site. We even explored the idea of video-streaming to allow real-time viewing on the Web. Currently, only the VA in White River Junction, Vt., receives a real-time video feed. (The VA also has an excellent weekly M&M, run by the chief medical residents.) A more conservative project is to archive the PowerPoint presentations in a viewer-accessible format. I can also envision linking the presentation to relevant studies, editing in transcribed comments after the presentation, or providing questions for self-assessment of comprehension of the material. But such projects will take more faculty time and resources than are currently available.
Directing M&M over 15 years has been a very positive experience for me. I have certainly learned a lot of medicine, like any participant. I have had the pleasure of working closely with residents. I have had a chance to influence the culture of the department— promoting the careful care of the individual patient, while celebrating medical knowledge in the service of that care. To me, the tradition of our M&M is one of holistic care—whole-person care that is informed by expert pathophysiological reasoning and evidence-based medicine, cognizant of social and financial issues, and always respectful of the ethical challenges inherent in caring for the ill.
Comments on M&Ms
The following insights regarding the ritual of "morbidity and mortality" conferences— known within medicine as "M&Ms"—were excerpted from interviews with and e-mails from assorted Dartmouth faculty members, residents, and current and former students.
Lorna Mayo, M.D., a fourth-year resident in internal medicine-psychiatry
Presenting a case at M&M lets patients teach providers how to be better doctors. It is a chance to make a patient who touched your heart touch the hearts and souls of others. M&M is a way for patients to reach out from the grave to humble and guide their doctors—to be immortalized in the knowledge they give physicians who might otherwise fail a similar patient in the future.
Larry Dacey, M.D., an associate professor of surgery and of community and family medicine
[The Department of Medicine's M&M] is the best conference in the Medical Center. I always learn something. It's like a detective story—an intellectual discussion on one case.
Ndidiamaka Onwubalili, a third-year medical student
You can always learn, and probably learn more, from the cases that don't go as well as you would expect. You'll never make the same mistake twice. Listen to the attendings, and you can learn a lot.
Michael Tamber, M.D., a third-year resident in internal medicine
While I was preparing a case for presentation, I picked up on some subtle aspects that I had not noticed while I was taking care of the patient. It was nothing that would have changed my initial management, but it did put a couple of things in a slightly different light.
Donald St. Germain, M.D., the acting chair of medicine and a professor of medicine and of physiology
The Department of Medicine is a large and diverse group, and this sharing of information in a nonthreatening environment is an important bonding activity. It helps us develop a sense of family, and therein lies some of the security that individuals find in offering their opinions. For our residents, I think seeing experienced clinicians engaged in complex problem-solving, and sometimes being humbled by the way the case develops, is very instructive.
Martha Graber, M.D., an associate professor of medicine (nephrology)
It's a great conference. It's the one thing in my week I wouldn't miss. The best cases are the ones where there's a postmortem and you get the answer. But I even learn when you don't get the answer. There's insight from collaborative discussion that you can't get just reading in a library by yourself.
Paul Testa, a fourth-year medical student
Medicine M&Ms for me as a medical student brought it all together. [A presentation about a patient he had cared for] was one of those teaching moments that I will always remember—the dialogue about the complexity not just of her illness but of her family's coping, of her history, and of her death. It was not simply clinical pearls to be memorized, but I watched clinical opinion leaders articulate their thought process as they worked through a case I had wrestled with—had feared—five months earlier.
Michael Alvarado, M.D., a fourthyear resident in surgery
[At other institutions' M&Ms], you squirm and come up with the right answers. Luckily, here it's more resident-friendly. You still stand up and pitch the case, but it's more of an open forum. It's more teaching than hammering the resident, like an oral exam. As a junior resident you're pretty busy. This really makes you focus on the patients.
Kathryn Kirkland, M.D., an assistant professor of medicine (infectious disease)
It provides a chance to learn how someone else might put together the same facts in an entirely different way because of their own knowledge base and experience. I think the way we have a lot of spontaneous discussion and interaction from many faculty, humor, and an emphasis on both what was done well and what could have been done better—all handled with a very light touch—really makes the conference work. I almost always walk away knowing something I didn't know before, or at least thinking about unanswered questions.
Pamela Kunz, M.D., a DMS graduate who is now a second-year resident in internal medicine at Stanford
At Stanford, M&Ms are attended mostly by residents and a few emeritus professors— unlike the M&Ms at Dartmouth, which are very well attended by active faculty. I was always impressed with the degree to which DMS faculty were involved in conferences, especially Grand Rounds and M&M.
Michael Stauder, M.D., a second-year resident in internal medicine
M&M is the best conference the Department of Medicine has. It allows you to reason through a case through the minds of many different attendings from many different specialties, taking in the best of what they have to say to optimize future care and medical decision-making.
Clifford Miles, M.D., a third-year resident in internal medicine
Our M&M conferences give the housestaff a chance to hear attendings reason out loud and contest each other's conclusions. Preparing our own presentation also allows us to think critically about a patient's entire course.
Peter Mogielnicki, M.D., a professor of medicine and former chief of medicine at the White River VA
The M&M conferences are extremely useful. The ones held at the VA are similar to the M&Ms at DHMC, but because they are smaller (attendance is about 50), they are a bit more intimate, and the discussion can at times be extremely frank and heated.
Sharon Johnston, a fourth-year medical student
One of the events that had a strong impact on me during my four years at DMS was an M&M at the VA. The case presented was a very difficult one involving end-of-life care and tough decisions made by the medical team. The attending physician began to cry during the presentation. As a student, I was horrified at seeing a physician cry. Then an other physician stood up and said he was sorry to the other physician—sorry for letting her down. He reminded us that we have one of the toughest jobs and we must support each other every day, especially when a colleague is having a difficult time. A lot can be learned at M&M—much more than the differential diagnosis and pathophysiology.
James Bernat, M.D., a professor of medicine (neurology)
[The most surprising thing about M&Ms], other than autopsy findings sometimes disclosing diagnoses not considered clinically, are those cases in which the total hospital and physician bill is presented. This is a useful reminder to us how expensive medical care is today.
Lin Brown, M.D., an associate professor of medicine (rheumatology)
The cases are usually unusual or have a twist, but there is always an effort to discuss general principles that are useful every day—the value of tests, the value of hindsight, tips on dealing with patients, reminders of diagnoses and how they are evaluated and treated.
Bethany Lovejoy, a third-year medical student
I enjoy hearing about input, new differential diagnoses, treatment options from representatives of infectious disease, pulmonary, etc. Their comments add ideas and insight not considered during the patient's actual hospital course.
Mary Margaret Andrews, M.D., an assistant professor of medicine (infectious disease)
AT DHMC, there's a collegial spirit of discussion. At other places, it's more like criticism when there's a disagreement.
Peter Spiegel, M.D., the chair and a professor of radiology
[At M&Ms during his residency in Boston], the residents were very much on the firing line. The atmosphere in Boston was more confrontational then. What's nice about DHMC is we're not a confrontational institution. We have a better learning atmosphere— you don't feel you're being set up.
Laura Carter is the associate editor of Dartmouth Medicine magazine. Some of the identifying details in this account have been changed in order to ensure patient confidentiality.
If you would like to offer any feedback about this article, we would welcome getting your comments at DartMed@Dartmouth.edu.
