Scrambled Sounds
By Laura Stephenson Carter
Photos: J.D. Denham (website)
Central auditory processing disorder is to the ear as dyslexia is to the eye. Just as dyslexics can see the words, but some letters get jumbled in their brains, those with CAPD can hear, but their brains aren't able to process some sounds. The disorder is often misdiagnosed, but that will change if DHMC's Frank Musiek has his way.
|
|
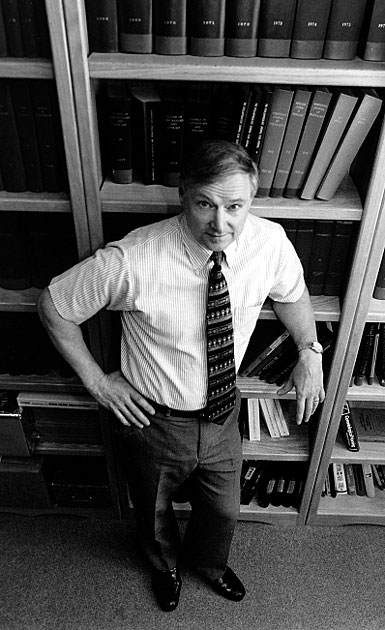
Dartmouth audiologist Frank Musiek has been working for over two decades to increase understanding of and awareness about CAPD. |
"Everybody's talkin' at me. Can't hear a word they're sayin' . . ."
Although these words to the hit song from the 1969 movie Midnight Cowboy refer to someone who felt overwhelmed, confused, and out of place in New York City, they could serve as the theme song for those who have a hard time comprehending the sounds around them. Imagine being able to hear words and sentences just fine, but when there are a lot of them and they're coming at you fast and faster, tumbling over each other until they're all jumbled up, you—or, more precisely, your brain—just can't sort out what they all mean.
That's what happens when you have CAPD—central auditory processing disorder. Few people have heard of the disorder, yet as many as three percent of school-age children may have it, according to Frank Musiek, Ph.D., director of audiology at DHMC and an international leader in the diagnosis and treatment of CAPD.
His eyes sparkle as he talks about research and therapeutic strategies that have pediatricians, audiologists, schoolteachers, speech pathologists, and learning disabilities experts flocking to his lectures, buying his books, and learning as much as they can about a condition that may be masquerading as attention-deficit/hyperactivity disorder (ADHD).
Normally the auditory regions of the brain, located in the left hemisphere, can process both simple and complex signals from the ears almost instantaneously, so the listener can interpret what the sounds mean. "Our auditory system works in a very unique way. Not only does it help us in terms of understanding—like me understanding you or understanding the primary speaker—but it also helps us to suppress the background noise that we don't want to hear," explains Musiek (whose name is pronounced "music").
But in someone who suffers from CAPD, auditory processing can be delayed or scrambled. Especially when there's background noise, the brain may try to process everything all at once and might never be able make sense of anything. "It's hard to distinguish foreground from background," explains Musiek, "so it presents a host of problems."
CAPD can occur in a variety of circumstances: if people have brain lesions; if someone has suffered a traumatic brain injury; in those with a history of chronic ear infections; in older adults, as a result of neurologic changes due to aging; or in children with learning disabilities such as dyslexia, developmental language disorder, or attention deficit disorder.
Because people with CAPD can usually pass ordinary hearing tests—where an audiometer emits assorted tones of varying frequency and intensity—the disorder frequently goes undiagnosed. "Often it's misdiagnosed as ADHD," Musiek says. In fact, CAPD may coexist with ADHD or with other learning disabilities.
Although CAPD is not considered a learning disability itself, Musiek and others suspect that it may be the underlying cause of some learning disabilities, especially those associated with language processing. "It's a prerequisite for a learning disability," he explains. "It's not one of the neuromechanisms related to learning—it's separate. It's a sensory process."
Musiek, who is a professor of surgery (audiology) and of medicine (neurology) at DMS, has spent most of the last 20-plus years trying to understand and identify CAPD as well as to develop ways of retraining the brain to overcome it. He, together with a number of other experts, has known for a while that the auditory and the language/reading/ speech centers of the brain are intertwined.
But if CAPD is tricky for even a specialist to diagnose, how can a teacher or a parent or a general pediatrician know when to suspect that a child might have CAPD?
"First of all, they don't follow directions well," Musiek says. "They miss assignments. They have poor phonetic learning, trouble with their vowels, reading skills below where they should be, [and] trouble spelling. They can't follow well when there's background noise. They often misinterpret what they hear. They say 'What did you say?' 'What was that again?'"
Musiek notes also that "there's a high correlation between CAPD and the inability to learn to play a [musical] instrument, because it requires similar skills." But while children who have CAPD may not be musically talented, it's their inability to learn basic academic skills in a typical classroom environment—filled with background noises—that has the most disturbing ramifications.
Learning vowels, for instance, is a challenge for any child but is particularly hard for kids with CAPD. "You have to be able to discriminate and identify vowels," Musiek says. "If you can't do that you are going to have problems in reading and in spelling."

|
|
Frank Musiek, shown here working with some of his auditory equipment, has developed an array of tests that he uses to diagnose CAPD and that he has also adapted to retrain the auditory system to mitigate the disorder's effects in patients—like Eric Hammond. |
But kids with CAPD may not even be able to hear the difference between long and short vowels. "If you look at the frequency spectrum of vowels, they're low frequency—ah, aah, ee," says Musiek. "Guess what also is low frequency—the ambient noise in the classroom. The ambient noise in classrooms across the United States averages 59 decibels. Most teachers saying vowels when they are teaching kids say them at about 60 decibels. Ambient noise in the classroom masks a lot of the subtle acoustic characteristics of vowels."
Musiek says that one of his patients, a nine-yearold boy, hadn't been able to learn vowels even though he had been trying for two years. "He knows what a long vowel is. He knows what a short vowel is. [He] just doesn't know what the sounds are because he hasn't heard them."
Being unable to hear or learn vowels has a snowball effect on learning to read. "If kids don't learn the appropriate way to identify phonemes in the English language, then what happens is they do it in reverse. They begin to learn the whole word and [then] figure out what the components are. That works great until they're in fourth or fifth grade and then the words become too complicated. The reading material is too complex and all of a sudden their reading [progress] levels off."
Sometimes CAPD is discovered in people who have not been previously classified as learning disabled. "We even see it at Dartmouth College—kids who have A's in all their subjects except foreign language, [where] they're failing. We've seen probably 20 of those kids, and all of a sudden it turns out that they have CAPD," says Musiek. "They are so bright that they've offset it [CAPD]. But when you have to start speaking a foreign language and hearing it all the time, it becomes very hard."
Nancy Pompian, Dartmouth College's student disabilities coordinator, has referred a number of students to Musiek. At Dartmouth there's a greater emphasis on speaking and listening in foreign language courses than in most high schools. Some students find it impossible to learn languages via this primarily auditory route. Musiek says he has diagnosed some of them as having CAPD.
But there wasn't much else he could do. Auditory training therapy at that age would have been very time consuming and difficult, and the students would have had to work extra hard to overcome years of "educational residue."
"Everybody does adapt some," explains Musiek. "Everybody—by the time they are 13, 14, 15 years old—has already developed some secondary neurons that are taking care of some things. Some of [the adaptations] are subliminal, they don't even know they use them."
The media has paid a lot of attention to the ADHD controversy lately: more kids are being diagnosed with ADHD and an alarming number treated with Ritalin. The American Academy of Pediatrics recently announced guidelines for diagnosing ADHD, to cut down on what many see as overdiagnosis of the disorder. But no one is paying much attention to CAPD.
Some of those ADHD cases might really be CAPD, Musiek believes. Although children with either ADHD or CAPD may show attention deficits, there are differences. The attention deficits of ADHD tend to affect more than one of the senses, while in CAPD the deficits are usually restricted to the auditory system. In addition, inattention, hyperactivity, impulsivity, and distractibility are the most prominent characteristics of ADHD. Children with CAPD, on the other hand, are most apt to have trouble processing incoming information, hearing amidst background noise, and following verbal instructions.
To determine whether a person has CAPD, Musiek conducts a battery of tests, individualized for each patient, including an ordinary audiogram to test peripheral hearing; an electrophysiological test (in which electrodes placed on the scalp record signals coming from different areas of the brain in response to auditory stimuli); and dichotic listening tests. The latter tests involve presenting different sounds to each ear simultaneously, while the patient pays attention to the sounds coming into a particular ear. There is a dichotic digit test, in which different numbers are fed to each ear; a duration pattern test, which uses different sequences of tones of varying lengths (long, short, long, etc.); and a frequency pattern test, with sequences of varying pitches (high, low, high, etc.). Sometimes Musiek uses other tests, too, such as compressed speech, where the dead space between words is taken out and the words come so fast that they are hard to comprehend, and filtered speech, where words are distorted because the frequency spectrum has been electronically altered.
|
Courtesy of Gordon Sherman, Ph.D., Harvard Medical School (website) |
After they are diagnosed with CAPD, patients have the option of coming to DHMC two or three times a week for therapy or working on the problem closer to home. Most choose to work at home or with learning specialists at their school. "What we usually do is formulate a home-school program," Musiek explains, "things that parents can do at home. Usually it's the speech pathologist in the school who helps coordinate it." Parents can make their own cassette recordings or use commercially available software.
Patients who choose to come to DHMC for their therapy are treated to listening exercises similar to the diagnostic tests—only many more of them. This auditory-skill training builds up the patient's temporal processing and listening-in-noise abilities.
One ear, usually the right, tends to be stronger, and part of the rehabilitation involves making the weaker ear work harder. "We turn down the intensity of the signal in the better ear, the strong ear, and we keep the intensity in the relatively poor ear at the same level," says Musiek. "What we force the system to do is to respond to the poorer side. We shut down the other by juggling the intensity, because . . . a loud-intensity sound will trigger more neurons to fire than a soft sound. If more neurons are stimulated on one side than the other, that particular ear-to-brain pathway is enhanced. And repeated enhancement of a certain pathway results in better function of neural elements in that pathway." He pauses. "You're not retraining the ears, you're retraining the brain."
It is possible for a child to outgrow CAPD when it's caused by a maturational lag, when "the auditory areas of the brain are not maturing . . . and then catch up," says Musiek. About 25 to 30% of children with CAPD have a maturational delay of their central nervous system. "But there could be other causes, such as when certain parts of the brain just—and these are subtle things—are not developed appropriately in the auditory areas. And then sometimes it's a pure neurologic problem. They have a seizure disorder, or they have an unusual type of neurological abnormality," he says. "But that's a rarity."
"It's pretty clear now that many dyslexics have auditory processing problems," Musiek says.
In the 1970s, Albert Galaburda, M.D., a researcher at Harvard, autopsied the brains of people who had been diagnosed with dyslexia and compared them to the brains of people who did not have any learning disabilities. He discovered nests of abnormal cells scattered throughout the auditory areas in the brains of dyslexics. Such "ectopic" cells didn't exist in people who were not learning disabled. Could these abnormal cells be interfering with the signals in the auditory region of the brain?
Today, Musiek is considered one of the leaders in CAPD research, is in demand as a consultant and lecturer on CAPD, has published or presented hundreds of papers on the topic, has written several books, and has developed some of the now commonly used diagnostic tests for the disorder.
"Frank Musiek is very well respected within the profession for his research and teaching," says Sharon Fujikawa, Ph.D., immediate past president of the American Academy of Audiology, the largest professional organization for audiologists in the country. "The growing interest in children with auditory processing disorders grows in large part from the research Dr. Musiek has conducted. He is [also] known for sharing his knowledge through innovative teaching methods that draw hundreds any time he presents at the Academy's conventions or elsewhere." Fujikawa, who is the director of audiology at the University of California at Irvine Medical Center, says that she has taken and enjoyed Musiek's popular three-dimensional course on the neuroanatomy of the brain.
CAPD was actually identified back in the mid-1950s. Ettore Bocca, an ear, nose, and throat (ENT) specialist in Italy, "discovered" central auditory processing. "He started to see patients in his hospital who complained of hearing difficulties and had trouble communicating," even though routine hearing tests showed that their hearing was normal, explains Musiek.
Bocca noticed that most of these patients were from the neurological wards, not the ENT wards. "He found out that a lot of them had damage to the auditory areas of the brain—to the temporal lobe," says Musiek. "That's when he started to call it what they called then 'central auditory testing.' He devised some tests that were more difficult, more involved, that tapped higher-order auditory processes. And lo and behold, when he got these patients back again and started to give them these tests, they started to fail them."
Then in the mid-1970s, an audiologist named Jack Willeford, at Colorado State University, noticed that some children with learning disabilities seemed to have the same kinds of comprehension problems experienced by people with brain lesions in the auditory system. The children were having trouble learning, reading, spelling, and hearing when there was background noise—yet they had normal audiograms. They were doing great in math and science, says Musiek, but they couldn't follow multistep directions and they misinterpreted messages.
|
Willeford "started to use some of Bocca's old tests and some new ones on some of these kids," says Musiek. "Lo and behold, he saw that they started to fail these tests. Then I got into it. We started to develop a lot of tests that we think were a lot better [than Willeford's tests]."
Musiek began working on CAPD in 1977, not long after he joined the DHMC Section of Audiology in 1975. "We were doing a lot of work on split-brain subjects [and] auditory perception, trying to figure out how the two hemispheres interrelated. And we've done a lot with stroke patients [and] with brain damaged patients to try to figure out what these mechanisms in the brain are doing when they're damaged. We used that knowledge to help us with kids with CAPD."
Musiek toiled in near-obscurity for the next 15 to 20 years, doing research on CAPD, developing diagnostic and treatment tests, and trying to educate others about the disorder. Yet few people—other than fellow audiologists and a smattering of language and learning disabilities specialists—were aware of his work. And even those who had heard of CAPD didn't really understand it.
Only within the last five to 10 years have any significant number of educators, learning specialists, and physicians begun to take notice of CAPD—at least partly because of growing awareness about the relationship between dyslexia and auditory processing problems.
Musiek thinks that ectopic, or misplaced, cells (the ones identified by Galaburda in the '70s) in the brain's auditory regions play a role in CAPD, too. His current research may shed more light on what's happening in the brain during both normal and abnormal auditory processing: he is part of a team of researchers doing functional magnetic resonance imaging (f-MRI) studies that he hopes will show which parts of the brain become active during central or other types of auditory tasks. At some point, f-MRIs may also be useful in determining whether the brain actually undergoes change as a result of the retraining process.
But although more people are aware of CAPD nowadays, there's still confusion about exactly what it is. Even DHMC neuropsychologist Art Maerlander, Ph.D., whose subspecialty is learning and attention disorders and who is quite familiar with CAPD (he conducts some of the diagnostic tests and refers patients to Musiek), admits that "I'm still trying to understand it myself." There seems to be "a lot of confusion still in the field," he adds, "which has hindered [Musiek's] work."
Musiek says he wishes the media would pay attention to CAPD. "If they [the media] would listen to the story, they would love it. But it's hard to do that, because it's something that you can't explain in five minutes."
"It's a sleeping giant," he adds. "Some day 60 Minutes will do a special on this—mark my words."
A CAPD success story
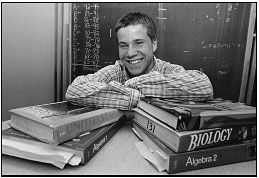
Eric Hammond, now a senior at Keene, N.H., High School has struggled with schoolwork all his life. Several years ago, he was growing more and more frustrated because he couldn't seem to learn as easily as other students. He was always asking classmates to repeat what the teacher had said.
And things were no better at home. He would constantly interrupt his mother, Janet Hammond, as she was talking to him. "Part of me thought he was being rude," she says. "Part of me questioned whether there was a learning problem."
It wasn't until he was in the eighth grade that Suzanne Jahn, the speech pathologist at Keene's middle school, suggested that Eric see Dr. Frank Musiek for an evaluation. Jahn suspected that Eric had either a language processing deficit or CAPD. "I wasn't sure which it was and wanted to rule CAPD out," she says. Luckily for Eric, Jahn was one of a growing number of learning specialists familiar with Musiek's work on CAPD. She had even been to some of his lectures at DHMC.
|
Eric and his mom went to see Musiek, who administered a battery of central auditory processing tests. Eric had to wear headphones and listen carefully as different words sounded simultaneously in each ear. Musiek would tell him which ear to pay attention to. The tests were difficult for Eric—and no wonder. It turned out that he had CAPD.
After Musiek explained CAPD to Eric and his mother, and described how it was probably affecting Eric's ability to learn, Eric says he felt a sense of relief. "It made me understand why it had been so hard for me to learn."
But the diagnosis was only the beginning. Eric would have to undergo intensive retraining of his brain if he hoped to overcome his auditory processing problem. He and his mother chose to come to DHMC for the therapy. That meant traveling to Lebanon two or three times a week, all summer, for auditory training. And Musiek wasn't even sure how successful the rehabilitation effort would be.
"He was 13 years old, and that was my first concern," Musiek says. "Most 13-, 14-, 15-yearolds aren't going to stick with these kinds of rather arduous therapy procedures. My second concern was that at that point in time I did not have a lot of experience with this particular protocol for therapy. It was something that I thought would work and that was based on pretty sound scientific principles, but I wasn't totally sure that it would work."
| |
|
Today, Eric Hammond (top) is headed for college—thanks to his school speech pathologist, Suzanne Jahn (left); to the support of his mother (below); and to DHMC's Frank Musiek. |
 Eric was determined, however. "I knew
it was going to be a lot of hard work," he
says, but he was willing to do it "if it was
going to make my schoolwork easier."
Eric was determined, however. "I knew
it was going to be a lot of hard work," he
says, but he was willing to do it "if it was
going to make my schoolwork easier."
So that whole summer before he started ninth grade, Eric and his mother made the hour-long drive from Keene several times a week. The retraining regimen involved having Eric listen to recordings that were similar to the diagnostic tests. Only this time his ears were bombarded with not just numbers and tones, but words and sentences, too— and, like the diagnostic tests, each ear was fed different sounds simultaneously, and Eric had to focus on what he was hearing in one ear and ignore the sounds coming into the other. Or he'd be asked to pay attention to both ears and report what he heard.The intensity of the sounds and their frequency would vary with each test, to train different processes.
The auditory retraining tests are very intense. "They made me tired," Eric says. "By the time I was done I was ready to go to bed." So he would sleep in the car on the ride back and do something fun when he got home, like play street hockey with his friends.
In addition to the therapy at DHMC, Eric did auditory exercises at home, too. "We used to listen to songs," his mom says. "Eric would have to focus on what the words were, then read the words out loud or to himself, then listen to the song again." The idea was for him to pay attention to that one thing—the words—and block out everything else. "He got way better at it," Janet Hammond says.
During his freshman year, Eric continued the exercises at home, worked with a tutor every day, and made sure that his teachers understood how to accommodate his learning needs. "I don't really know if I noticed the change," he says, but his mother and tutor did. "My grades got better," he adds. In fact, Musiek still recalls a call he got from Janet Hammond. "The day he [Eric] got his report card, she called me. She said she couldn't believe it, that he was on the honor roll for the first time ever."
The improvement in Eric's schoolwork wasn't solely because of the auditory retraining. He has continued to work with a tutor throughout high school, and his teachers have been educated about how he learns best. For instance, he can't listen to a lecture and take notes at the same time. So after each class, either he borrows notes from a classmate or the teacher gives him a copy of the lecture notes. He also takes exams in a separate room so as not to be distracted by background noise.
"Eric is a great kid, who despite his learning disability has remained determined not to let his disability get the better of him," says Charles Hansel, Eric's guidance counselor and the assistant coach of Keene's varsity hockey team, on which Eric played goalie. "A lot of kids in his situation would give up. He's exactly the same in hockey. I've never come across a kid who's so motivated."
Eric may be motivated both academically and in hockey, but he admits that "it was frustrating . . . to work so hard and have so much trouble learning." Understanding the underlying cause of his problems, retraining his brain so it will process information better, and figuring out how to adjust his environment to facilitate learning have helped. So much so that this fall, Eric will be attending New Hampshire College in Manchester.
Laura Carter is the associate editor of Dartmouth Medicine magazine.
Back to Dartmouth Medicine Summer 2000

 These diagrams of the left (top) and
right (bottom) sides of the brain show,
with dots, the areas where ectopic cells
have been identified in the brains of
dyslexic patients. Musiek thinks that
similar clusters of abnormal cells may
be responsible for CAPD as well.
These diagrams of the left (top) and
right (bottom) sides of the brain show,
with dots, the areas where ectopic cells
have been identified in the brains of
dyslexic patients. Musiek thinks that
similar clusters of abnormal cells may
be responsible for CAPD as well.