Mountain Aerie
By Paige Wickner and Fordham von Reyn, M.D.

|
|
This image is reproduced from a 1909 postcard featuring a hand-tinted photograph of the administration building at New Hampshire's Glencliff Sanatorium. |
Today's quarantining of SARS patients recalls an earlier era, when Americans suffering from a common and oftenfatal respiratory illness—tuberculosis—were isolated from society in sanatoriums. New Hampshire residents with TB were cared for at this serene mountainside retreat.
Every year, thousands of people— including any number of Dartmouth students and faculty members—make the trek up the eastern flank of New Hampshire's Mt. Moosilauke. Probably few of those hikers know that on the other side of the mountain lies a nearly 100- year-old health-care facility. The same alpine air that has lifted the spirits of many an outdoors enthusiast or overworked medical student has also been casting its healing powers over patients sequestered on the storied peak's southwestern side.
From the mountain's 4,802-foot summit, it's a four-mile walk down the Glencliff Trail to the serene and spacious grounds of the former Glencliff State Sanatorium, now the Glencliff Home for the Elderly. In the era before antibiotics were available to treat tuberculosis, Granite Staters with this often-fatal disease would seek admission to Glencliff for the restful mountain "cure." They arrived with a mixture of hope and resignation: hope that they would be among those who survived and resignation that they faced long months, or perhaps even years, of forced inactivity and of isolation from their families and friends.
"The San," as many residents of the nearby towns of Glencliff and Warren still call the facility, opened in the summer of 1909. It treated more than 4,000 TB patients during its first 50 years, admitting from 50 to 100 new patients each year.
One such patient was Ruth Bagley. In 1945, the 23-year-old Bagley was a newly commissioned first lieutenant in the Army Nursing Corps, scheduled to ship out any day for London. It was an exciting time for a young woman from a small town in northern New Hampshire who had never been outside of New England. But then, with all her bags packed and her departure imminent, she was told that her chest x-ray was abnormal. That she had tuberculosis. That she would not be able to go overseas with her unit.
|
|
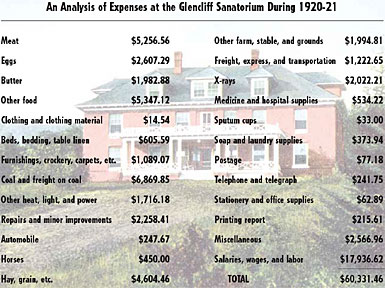
The state legislature funded most of Glencliff's annual operating cost. Above is an accounting of its expenses about a decade after the facility opened—a year in which the average daily census was 68.61. Some patients stayed there for years. The postcard below, which depicts "The San" on its front, was sent in 1912 from the Warren Summit post office, which served the facility. |
She was devastated at being left behind and at facing a prolonged period of enforced rest to improve her chance of surviving the disease. After initial treatment in an out-of-state army hospital, she managed to wangle a transfer to the Glencliff Sanatorium in her home state. She described her arrival on the slopes of Mt. Moosilauke as follows: "I was exhausted, and the Glencliff doctor came in with me, took hold of my arm, and said 'You're in the right place; you're going to get well.' I went to sleep for 24 hours."
|
Bagley stayed at Glencliff for more than two years—a period lost from her young life—and eventually left (against medical advice) when she felt that she had recovered her strength and that the cure had been successful.
The idea that rest, mountain air, and adequate nutrition would have a salutary effect on the outcome of tuberculosis emerged gradually, based on personal anecdotes and unscientific ideas about the nature of the disease. The sanatorium (the word comes from the Latin sanare, meaning to heal) movement began in 1791, when a London physician noticed that fishermen did not seem to be susceptible to tuberculosis of the cervical lymph nodes, a form of the disease known as scrofula. He established the Royal Sea Bathing Infirmary for Scrofula at Margate, which provided a season of open-air treatment and sea-bathing for those with tuberculosis.
Travel to a more healthy climate was also recommended, for those able to afford it, as exempli- fied by the poet John Keats's escape from dank England to sunny Rome in 1820, not long before he died from tuberculosis.
By the middle of the 19th century, TB accounted for a quarter of all deaths in Europe. In 1849, Hermann Brehmer established an open-air treatment center in the mountains of Silesia, based on his recovery from tuberculosis after a trip to the Himalayas, where he had been exposed to sun, air, cold, and plentiful food. Sanatoriums were subsequently built throughout Europe, where they often catered to a wealthy clientele able to afford these mountainside spas.
In 1882, German biologist Robert Koch identi- fied Mycobacterium tuberculosis as the cause of the disease. The bacteria, which are transmitted via airborne droplets from coughing, can lead to infection in the lungs of susceptible individuals. Most people contain the bacteria in a latent state and do not develop symptoms. In some people, however, the infection progresses to active (or reactivated) TB and the formation of large cavities in the lungs. But despite Koch's discovery of the disease's causative mechanism, there was still no treatment other than the rest and fresh air offered in sanatoriums.
The sanatorium movement was imported to the United States in the late 1800s by Edward Livingston Trudeau. He had developed tuberculosis in medical school—an occupational hazard that affected as many as one in five doctors and nurses in training during the 19th and early 20th centuries. Trudeau recovered from his initial episode of tuberculosis during medical school but then suffered a relapse while he was practicing as a surgeon. In 1873, at the urging of friends, he traveled to the Adirondacks.
His health improved there, and he became convinced that fresh mountain air had a beneficial effect on the natural history of tuberculosis. He built the first American sanatorium at Saranac Lake, New York, in 1884. There, and later at Glencliff and other remote locations, the mission of sanatoriums in the United States was to treat patients who had reasonable prospects of survival from tuberculosis, regardless of their ability to pay.
| |
|
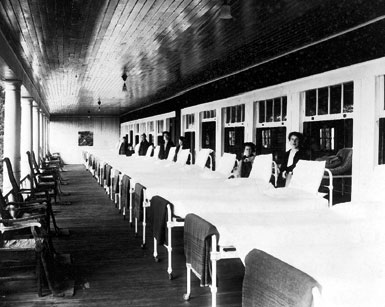
The photo above, taken in the early 1930s, depicts one of the open-air porches where Glencliff patients slept year-round. Below left, Ruth Bagley was a first lieutenant in the Army Nursing Corps during WWII when she was diagnosed with tuberculosis and became one of the more than 4,000 patients treated at Glencliff—below right—during its first half-century of operation. | |

|

|
Rigorous scientific support for the benefits of rest and fresh air on the natural history of tuberculosis, however, was never provided. Trudeau justified the concept with a famous study at Saranac Lake in which 10 rabbits were inoculated with tubercle bacilli and then divided into two groups: one in which the animals were allowed to roam free on an island with fresh air, sunshine, and plentiful food, and another in which the animals were kept in a trench and underfed.
The small number of animals in the study and its multiple variables would not be likely to pass peerreview scrutiny today, but Trudeau believed that the 80% survival rate in his "sanatorium" group, compared with a 20% survival rate in his control group, proved his point.
In New Hampshire, the state legislature authorized construction of a sanatorium in 1901, a year when the state's annual death rate from tuberculosis hit 194 per 100,000 and tuberculosis was the most common cause of death for persons aged 20 to 40. Had tuberculin skin testing been available at the time, virtually every adult would have tested positive—an indication of either latent infection or active disease.
This is in stark contrast to the current situation in New Hampshire. Today, the annual incidence of tuberculosis is 1.6 per 100,000, and fewer than 10% of DMS students have positive tuberculin skin tests (and most of those who do are foreign-born students from countries where tuberculosis is still common). Dartmouth-Hitchcock Medical Center admits only between one and four patients a year with active tuberculosis, and most of them recover after six months of treatment. Dartmouth medical students and residents are more likely to see patients with systemic lupus erythematosus, a chronic inflammatory disease, than with tuberculosis.
The New Hampshire State Sanatorium was located at Glencliff because the site's elevation of 1,650 feet would provide the fresh mountain air that was then thought to be therapeutic for tuberculosis patients. Construction on the facility was completed in the summer of 1909, and the first patient was admitted on September 14 of that year. Dr. John M. Gile, a professor of clinical surgery and later the dean of Dartmouth Medical School, was the first consulting surgeon at the sanatorium, and Dr. Elmer Carleton, also a member of the DMS faculty, was the consulting laryngologist. Most patients came from the major industrial centers in southern New Hampshire, such as Manchester, Concord, and Nashua, but any resident of the state identified as having active tuberculosis would be considered for admission.
Admission required that the patient first be seen by a designated practitioner in Claremont, Dover, Keene, or Manchester or at the sanatorium itself. These physicians were asked to consider whether the applicant presented "a reasonable prospect of improvement or cure" before they referred the patient to the superintendent of Glencliff for admission. Patients with an unfavorable prognosis were usually turned down, though sometimes they would be accepted if it was thought that small children in the patient's home were at risk of infection.
In general, Glencliff did not accept children, although the cutoff for adulthood at the time was 14 years. So-called "pre-tuberculous" and tuberculous children were treated at another New Hampshire facility, the Pembroke Sanatorium, beginning in the early 1920s.
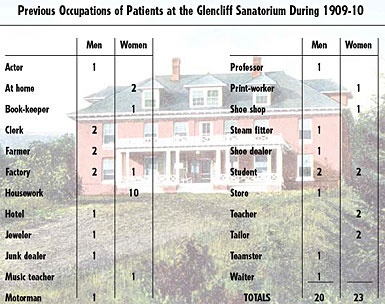
Glencliff's patients came from all social classes and all professions and included doctors, hospital superintendents, factory workers, steamfitters, and junk dealers. For many patients, their stay lasted years, sometimes even decades. A Chinese exchange student at Dartmouth stayed for two years. One patient remained at the sanatorium for 23 years.
In the early 1900s, Glencliff was a self-sufficient community, designed to maintain the isolation that was part of the sanatorium concept. Its medical facilities included a hospital unit, an open ward, an x-ray facility, an operating room, and a microbiology laboratory. The campus encompassed 500 acres and included a farm with pigs and cows and a vast vegetable garden. The institution made its own maple syrup, pasteurized its own milk, and sent summer vegetables to be canned at the New Hampshire State Hospital in Concord. Electricity, water, and sewage disposal were all provided by the nearby town of Glencliff. Coal was brought to the base of the mountain by train until the railroad was discontinued in 1952. The sanatorium even had its own shortwave radio station.
|
|
Glencliff's patients came from all walks of life. The data above, from the facility's first biennial report, shows the previous occupations (spelled exactly as in the report) of its original complement of patients. The advertisement below, from an 1895 newspaper published in Glencliff, suggests the impact that TB (referred to here by its old name—consumption) had on society. |
The institution was funded by the state legislature, and the trustees were required to submit biennial reports detailing its programs, staffing (for example, there was a 1:8 ratio of nurses to patients in 1936), and costs (which were $12 per patient per week in 1909 and $16 per patient per week in 1938). Glencliff also received various private do ations, including a Victrola given one year by a famous actor. Many employees were from the towns of Glencliff or Warren. For many workers, the sanatorium became their home. Guy Labounty, who worked as the head of the farm for 20 years, recently reminisced: "We raised our kids on the farm up there. . . . We had a beautiful house. . . . We got milk and occasional pork from the farm—maybe the tip of a pig's head—and had our own garden for other things. The kids went to school nearby; they lived there most of their lives."
|
The public's perception of patients with tuberculosis had evolved considerably by the time Glencliff opened its doors. In the early 19th century, tuberculosis was viewed as a romantic affliction, since it had been the cause of death of several young poets— including Keats and Shelley. It was considered a fashionable way to die, a disease bestowed on the talented and artistic.
| |
|
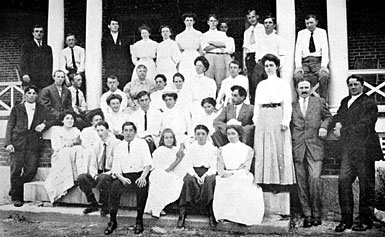
"A group of patients" was the legend on the photo above in Glencliff's first biennial report, published in 1910. In that year, the facility included the building pictured on pages 42 and 43; two wards, including the one pictured below left; and several outbuildings, including the heating plant pictured below right. Later additions included a bakery, an infirmary, and a recreation hall. | |

|

|
As the industrial age emerged, tuberculosis became associated with factory work, malnutrition, crowding, and poor living conditions. The disease became an embarrassment and usually made one ineligible for marriage or unsuitable for hire. The attitude toward the patients at Glencliff was varied. Many employees did not worry about working there, while a few were terrified. Clifford Ball, who worked as a dishwasher and then a housekeeper from 1931 to 1970 says, "When I first went there, I was ready to quit the next day. But the next day I put it off till the next day, and the next thing I knew I had been there for nine years. I was scared about it at first. If I had the least little sniffle or cough or something, I thought maybe I had tuberculosis. I escaped it, I guess, and now I'm 90 years old."
Bertha Keysar, a nurse at Glencliff from 1960 to 1982, recalls that "People would say to me, 'Aren't you scared to go to work?' I said, 'No, I know what those people have got. I go to a restaurant and I'm sitting beside somebody and I have no idea what they have.'"
Many patients felt stigmatized by the disease, and these feelings lasted beyond their stay at Glencliff. "I knew enough about tuberculosis to know that it was infectious and that people were afraid of it," one former patient says. "You felt uncomfortable, especially when you were out with other people, even if you just had a negative checkup. Two of the girls I went to high school with in Pittsburg [N.H.] both had tuberculosis and were treated at Glencliff. Their father used to take me and other girls in town to visit them. Since they both got well and went home, there was a good precedent in Pittsburg. I sometimes felt isolated while I was there, but not usually, because it was a friendly place. It was your own little world, and it was a good world except when you thought you were on the road to recovery and found you still had a positive sputum. It wasn't that bad for me, but probably worse for the mothers and fathers and husbands waiting for people to come back. I was young and felt that some of my life had been taken away from me."
For some, being diagnosed with tuberculosis was an embarrassment not only because of the shame of having a contagious disease but also because it was most common among the urban poor—which explains why most of the Glencliff patients came from Manchester and Concord in the more urban southern tier of the state. The same patient recalls a friend at Glencliff "from Boston, a member of the Boston 500, 'the elite.' She told me that her family considered tuberculosis a disease of the masses, and she was embarrassed. She had one aunt who visited her, but was there a long time before her mother finally visited once."
But despite the widespread fear of tuberculosis at the time, both staff and townsfolk would attend weekly movie nights in the sanatorium recreation halls, where they would all sit together without separation, masks, or other precautions.
|
In the early years of Glencliff's existence, the treatment of tuberculosis consisted of fresh mountain air, bed rest, and a healthy diet. The patients were placed on large screened porches throughout the year—bundled up in blankets with hot water bottles and special lamps to keep them warm during the cold northern New Hampshire winters. Sedentary activities were permitted. Since nutrition was also thought to be a major factor in recovery from the disease, weight gain was taken as a sign of improvement. In describing the type of patient likely to require readmission, the 1913-14 trustees' report demonstrates the faith that was placed in the basic sanatorium formula: "The expatient who fails to avail himself of these hours for rest, open-air life, and open-air sleeping . . . is the person who is certain to be readmitted to the sanatorium."
New methods of treatment were introduced over the years, with surgical approaches appearing in the 1930s. The challenge was how to prevent the lung cavities that are characteristic of advanced TB from continuing to expand and, often, leading to death. Animal studies and anecdotal reports of improvement in patients with advanced tuberculosis who developed a spontaneous pneumothorax—a condition in which air enters the pleural space, between the membranes on the outside of the lungs and the inside of the chest wall—suggested a potential benefit from lung-collapse therapy. The therapeutic injection of air into the pleural space to collapse the diseased lung (a procedure known as an artificial pneumothorax), gained acceptance in the 1920s and 1930s. "San" records indicate that this approach was tried briefly at Glencliff in 1922, suspended for reasons that the historical record does not make clear, and then resumed on a larger scale in 1930. Thousands of artificial pneumothorax treatments were performed by the staff at Glencliff— with "refills," or repeat pneumothorax treatments, done at set intervals for between two and four years and fluoroscopy performed after each instillation. Case records in the United States suggested that such treatment was effective in about a third of patients, especially in those who had not responded to rest alone and whose disease was limited to one side of the lung.
|
|
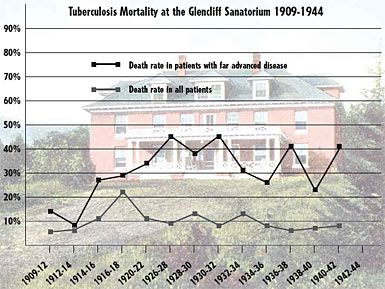
The graph above shows the devastating death rate from TB among Glencliff patients—in some years, close to 50% in those with far advanced disease. Below is a present-day photograph of the 1909 building depicted above; the long porch has been removed, but the building is otherwise unchanged—as is the serene setting for what is now the Glencliff Home for the Elderly. |

|
By 1932, more invasive surgical procedures were being used to treat tuberculosis at Glencliff, specifically extrapleural thoracoplasty. This procedure involved the removal of several ribs to bring the chest wall down to the lung and thereby collapse the tuberculous cavity. Patients were instructed to lie on a pillow to push the chest wall against the lung after the ribs had been removed. At least one Glencliff patient subjected to this treatment says that this procedure was very painful and sometimes led to temporary addiction to opiates. Thoracoplasty was observed to reduce the one-year mortality of cavitary tuberculosis from 80% to between 14% and 27%.
Phrenic nerve avulsion, or crushing a nerve to paralyze the diaphragm, was also introduced at about the same time at Glencliff. Lorraine White, a nurse and operating room assistant who worked in the sanatorium hospital from 1949 until 1970, describes another method of collapse therapy known as plombage thoracoplasty: "Plastic balls were placed in the chest, left in for some time to collapse the lung, and then later removed."
Many of the surgical collapse procedures were performed in the single operating room at Glencliff and were done by physicians from Dartmouth, as well as by two surgeons who traveled up periodically from Boston. Dr. Dawson Tyson from Dartmouth performed phrenic nerve resections, thoracoplasties, and extrapleural pneumonolyses during his involvement with the statewide program for the surgical treatment of tuberculosis in the early 1940s. During this time, Glencliff also used Mary Hitchcock Memorial Hospital's pathology and autopsy services, as well as consulting with other specialists from Dartmouth.
Beginning in 1936, intramuscular gold injections were also tried briefly, but were soon discontinued due to the treatment's toxicity and the dif- ficulty of obtaining this German preparation during World War II.
During the pre-antibiotic era at Glencliff, death was a common outcome for patients with chest x-rays that showed the distinct cavities indicative of far advanced disease. The annual reports filed by the institution include statistics on admissions, disease classifications, and deaths—from which it can be calculated that overall mortality rates during the period from 1909 to 1944 ranged from 5% to 22%. An average of 20 patients a year had far advanced pulmonary tuberculosis, and the mortality rate in that group ranged most years between 25% and 45%. And the death rate remained high among patients with far advanced disease even after the introduction of lung-collapse therapy.
But the outlook for patients with tuberculosis changed dramatically after the 1944 discovery of streptomycin, the 1946 discovery of paraaminosalicylic acid (PAS), and especially the 1952 introduction of isoniazid.

| |
|
Considerable effort was put into keeping the Glencliff patients occupied. The photo above shows the recreation hall as of the early 1930s. Below left are participants in an occupational therapy class during the early 1920s, with raffia furniture they had made for the reception room of the infirmary. Sometimes, however—as at the lower right—patients simply rested in the open air. | |

|

|
Treatment began to shift from sanatorium con- finement and surgery to inpatient and outpatient chemotherapy. But Bertha Keysar recalls difficulties with early forms of PAS: "It was a liquid, and you had to have an iron stomach to tolerate it." White remembers that even though "the drugs made quite a . . . difference, patients still remained one or two years . . . depending of the severity of the tuberculosis and how they reacted to the drugs."
By 1970, other potent new drugs, including rifampin, were also available. That year, Glencliff sent its last active tuberculosis patient to Mary Hitchcock Hospital, ending the sanatorium movement in New Hampshire. The once-flourishing U.S. network of 420 sanatoriums was soon virtually abandoned. Many of the hospitals were eventually converted to other uses, though some were left empty for fear of contagion.
A resurgence of TB in the 1980s was due in part to the HIV epidemic—patients who are HIV-positive are at greatly increased risk of developing active tuberculosis—and also to the dismantling of public-health programs and spe cialized treatment centers. Dr. Dixie Snider of the Centers for Disease Control and Prevention, reflecting on the end of the sanatorium movement, observes: ┼gIn most places, unfortunately, an effective network of outpatient clinics was not substituted for the sanatorium.┼h
Long gone were the public awareness campaigns that pervaded New Hampshire┼\ involving play-writing contests, health crusades, and yearly slogans promulgated via poster campaigns┼\such as ┼gEarly Discovery, Early Recovery┼h and ┼gProtect the Family Circle┼\ Get a Chest X-Ray.┼h
In 1970, the Glencliff Sanatorium was converted into the Glencliff Home for the Elderly. Through the efforts of Sandra Knapp, Glencliff┼fs administrator from 1979 through 2002, and the current administrator, Todd Bickford, many of the unique architectural features of the original facility have been preserved. The main patient building still has its floor-to-ceiling windows that admit ample light and the sturdy columns that used to support the screened porches which were used for the open-air treatments (these spaces have now been framed in, however, to create additional patient rooms).
Glencliff continues to generate its own electricity, using a system of pipes running from a pond on the side of the mountain to a turbine several hundred feet below. The facility┼fs connection with Dartmouth continues as well; Dr. Thomas Oxman, a professor of psychiatry, serves as the medical director for the home and travels to Glencliff weekly with DMS students.
Even today, the drive from the busy Dartmouth- Hitchcock Medical Center campus to the quiet mountainside retreat at Glencliff transports visitors to another place and time. There is still an undeniable, though indefinable, sense of serenity and health that washes over you the minute you open your car door at Glencliff. The venerable, wellsited brick and clapboard buildings; the expansive views toward Vermont; the mountain breezes; the friendly and collegial staff; and the peaceful, self-contained campus atmosphere recall a different, distant era in our approach to health.
Paige Wickner is a DMS '03 and plans to do a residency in internal medicine at Brown University. Ford von Reyn is chief of infectious disease at DHMC and a 1969 graduate of DMS. Among sources they used in researching this article were The White Plague by Rene and Jean Dubos; "Tuberculosis Then and Now: A Personal Perspective on the Last 50 Years" by Gordon L. Snider, in the February 1997 issue of the Annals of Internal Medicine; and "History of the Sanatorium Movement" by Anne L. Davis, in Tuberculosis, edited by William Rom and Stuart Garay. Appreciation is extended for help in locating illustrations for this piece to Kristin Rose, for the loan of the photos of her mother, Ruth Bagley; to Grover Libby of the Warren, N.H., Historical Society; to Todd Bickford, Sandra Knapp, and Robyn Raycroft of the Glencliff Home for the Elderly; and to Dr. Edwin Blaisdell.
If you would like to offer any feedback about this article, we would welcome getting your comments at DartMed@Dartmouth.edu.
