Economic cost of osteoporosis gains national attention
Osteoporosis, the most common of all bone diseases, affects millions of Americans and costs billions of dollars a year but is only beginning to get the attention it deserves, believes a Dartmouth researcher. Anna Tosteson, Sc.D., an associate professor of medicine and of community and family medicine, has been studying the economic impact of the debilitating disease for more than a dozen years.
Experts: Recently, Tosteson's work was factored into the recommendations of a national panel that was charged with evaluating the latest scientific information on the disease. She was one of several national and international experts brought in to advise the National Institutes of Health (NIH) Consensus Development Conference on Osteoporosis Prevention, Diagnosis, and Therapy.
Considering the economic implications of a disease is a relatively new venture for NIH consensus panels, about half a dozen of which are convened each year. But with health-care providers under pressure to maximize limited resources, there is increasing recognition of the need for informed research concerning the cost-effectiveness of different prevention and diseasemanagement methods.
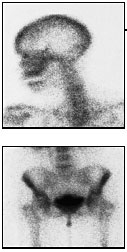
Osteoporosis—which comes from the Greek for "porous bone"—is characterized by a decrease in bone density, which results in an increased risk of fractures. Although some thinning of the bones accompanies aging, abnormal bone loss can have serious consequences. The disease itself has no obvious symptoms; it is the threat of broken bones that makes it so devastating. Fractures, especially of the hip, can result in chronic pain, disability, and even death. Studies show that 80% of women 75 and older would prefer death to a bad hip fracture that requires placement in a nursing home.
The prevalence of the disease is on the rise. Currently, at least four to six million women and one to two million men have osteoporosis. But, says Tosteson, "because the elderly population is expected to double by the year 2025, if nothing is done the number of persons affected by osteoporosis will dramatically increase.
"From a public health and policy perspective," she adds, "these projections make it imperative that we understand the overall costs of osteoporosis and identify economically sound approaches to osteoporosis prevention and treatment."
Preventable: The good news about osteoporosis is that it is largely preventable. An adequate intake of calcium and vitamin D are crucial to preserving bone mass throughout life, according to the NIH consensus panel. The National Osteoporosis Foundation recommends taking at least 1,200 mg of calcium and 400 to 600 units of vitamin D a day. Regular weight-bearing exercise can also help prevent osteoporosis and may reduce the risk of falls in older individuals.
A widely held misconception about osteoporosis is that it only affects postmenopausal white women. Although males and non-white women are at less risk, the disease knows no racial or gender barriers.
 "Osteoporosis occurs in all
populations and at all ages and is
a devastating disorder with significant
physical, psychosocial,
and financial consequences,"
said the consensus panel's chair,
Anne Klibanski, M.D., a professor
of medicine at Harvard.
"Osteoporosis occurs in all
populations and at all ages and is
a devastating disorder with significant
physical, psychosocial,
and financial consequences,"
said the consensus panel's chair,
Anne Klibanski, M.D., a professor
of medicine at Harvard.
In her presentation to the panel, Tosteson outlined two forms of research used to do economic evaluations: cost-of-illness studies and cost-effectiveness studies.
Studies: Cost-of-illness studies estimate the total economic burden of a disease in a defined population. For osteoporosis, Tosteson says, the cost is $16 billion per year and climbing. And, she adds, $16 billion is a conservative figure, since it doesn't con sider less quantifiable costs such as diminished quality of life and increased pain and suffering. By 2025, osteoporosis could cost the nation upwards of $45 billion a year. "With the size of the elderly population set to approximately double in 25 years," says Tosteson, "the $45-billion figure is not inconceivable."
In contrast, cost-effectiveness analysis (CEA) assesses the relative value of the available prevention and treatment interventions. "The rationale for CEA is that with limited resources, each expenditure should provide a benefit worth its additional cost," says Tosteson. Although they are controversial as a method for establishing treatment guidelines, such studies can be valuable as a way to highlight the most efficient opportunities for prevention and treatment, she explains.
Resources: "Cost-effectiveness information is rarely or never used as the sole determinant for health-care resource allocation decisions," says Tosteson. "The point of cost-effectiveness analysis is to highlight our best opportunities for improving health and to allow us to make the most of our limited resources."
Tosteson, who is affiliated with Dartmouth's Center for the Evaluative Clinical Sciences, is the principal investigator of an NIH-funded study of osteoporosis. Her early work focused on the cost-effectiveness of bone density screening, and her recent research has involved the health and economic consequences of fractures due to osteoporosis.
Sara Connolly
If you would like to offer any feedback about this article, we would welcome getting your comments at DartMed@Dartmouth.edu.
