DMS and Thayer team up to test new imaging methods
Although mammography is credited with saving thousands of lives through the early detection of breast cancer, it remains one of the most challenging of all radiological procedures. Conventional mammography, which uses x-rays, must sometimes be coupled with ultrasound in order to distinguish cysts from tumors. Even so, the process is not well suited to younger women, because they tend to have much denser breast tissue.
But some other options are now on the drawing board. Just over a year ago, the National Cancer Institute awarded nearly $7 million to Dartmouth to explore four new techniques for breast imaging. The principal investigator for the effort is Keith Paulsen, an associate professor at Dartmouth's Thayer School of Engineering and a 1986 graduate of its Ph.D. program in biomedical engineering.
|
|
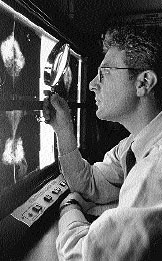
Radiologist Steven Poplack is overseeing the
clinical aspects of developing four new imaging
techniques to augment or replace mammography;
the project is funded by a nearly $7-million
grant from the National Cancer Institute. |
Similarities: The four new imaging techniques make up four subprojects of the grant. There are a couple of similarities among the subprojects. First, all four draw heavily on central computational capability. The output from either conventional mammography or ultrasound is in the form of a photographic image that can be interpreted by a radiologist. But the raw data from the new imaging techniques is too diffuse for photographic imaging, and so it needs to be mathematically re- fined and enhanced. In addition, all four of the techniques are so new that most of the equipment and instrumentation that they require has had to be custom-built in labs at the engineering school.
Four subprojects: Brian Pogue of the Thayer School is heading up a subproject that is attempting to use optical tomography in combination with spectroscopy. Tomography, a process that is already widely used in radiology (the "T" in CT scan stands for tomography, for example), provides information on a slab of tissue in the body.
The hope is that this technique can avoid the problem caused on a conventional mammogram by overlapping structures in the breast. The new technique involves measuring the propagation and scattering of light through the breast in a slice-by-slice fashion. The process uses monochromatic light— that is, a single wavelength of light—in the near-infrared range, which makes it possible to measure the hemoglobin concentration within the tissue. Breast tumors need to develop their own blood supply through a process called angiogenesis in order to survive. The hope is that the enriched blood supply to a tumor can be visualized spectroscopically as an increase in hemoglobin concentration, and then mapped to a specific location within the breast. This technique has already been used in a preliminary fashion, with encouraging results, on about 35 women.
The other three techniques are similarly cutting-edge. John Weaver, Ph.D., an associate professor of radiology, is applying the technique of magnetic resonance elastography to tumor imaging. This method, which is only about five years old, depends on measurements of the displacement of tissues in a magnetic field, from which one can infer the stiffness, or hardness, of the tissue. Malignant tumors are usually less elastic, or harder, than either normal breast tissue or benign tumors.
Alexander Hartov, Ph.D., a research assistant professor of surgery, is working with a process called electro-impedance spectroscopy, which explores the ways in which electrical current or voltage is conducted through breast tissue.
And Paul Meaney, Ph.D., of the Thayer School is working on a method that uses microwave propagation through tissue to produce spectroscopic images. This technique has now been tested in about 15 patients.
At this point, it appears that the time involved for an examination with any of the new techniques is comparable to that of conventional mammography. It is possible that the new methods will offer some economies over mammography, however, since they may turn out to be less operator- dependent.
Compression: In addition, some women complain of discomfort during conventional mammography —since current technology requires the breast tissue to be compressed between two plates —so the fact that none of the four new methods involves compression of the breast is seen as a benefit.
All the new techniques will, of course, be compared with conventional mammography and ultrasound. In addition, the researchers will determine whether the new techniques prove to have synergistic effects when used in combination with conventional methods. Thus the new techniques may end up augmenting rather than replacing the older ones.
The clinical aspects of the project are being overseen by Steven Poplack, M.D., an assistant professor of radiology. He explains that there are no satisfactory animal models on which to test these techniques because each is critically dependent on the unique composition and geometry of the human breast. However, the investigators have established the safety of the new techniques through simulations and tests on phantom and surrogate human tissue as well as in volunteer subjects. Both in theory and in practice, there appears to be no risk to humans.
Enrollment: Eventually, the researchers plan to enroll 150 patients in the project. Of those, half will come from a group in which a biopsy has been recommended on the basis of mammography or ultrasound. For this group, there will be immediate biopsy evidence to confirm or refute the findings of the new techniques. The other 75 study participants will serve as controls— as will the opposite breast in the biopsy group, since the vast majority of these women will have a biopsy on a single abnormality in only one of their breasts.
In the meantime, preliminary studies are now under way to define with each of the four new techniques the normal range of images in women of different ages and breast densities. The researchers are also using the new methods to record the appearance of breasts with benign abnormalities that were established with conventional methods. Such a database of experience has been accumulating over more than 20 years for mammography, and now one must be built for the new methods.
Roger Smith, Ph.D.
If you would like to offer any feedback about this article, we would welcome getting your comments at DartMed@Dartmouth.edu.
